Kidney transplantation from brain-dead donors with hepatitis B or C in South Korea: a 2015–2020 korean organ transplantation registry data analysis
Hoonsung Park1, Hanyoung Lee2, Seungmin Baik3, Myoung Soo Kim4, Jaesoek Yang5, Jong Cheol Jeong6, Tai Yeon Koo7, Deok-Gie Kim8, Jae-Myeong Lee2.
1Department of Trauma Surgery, Uijeongbu St. Mary’s Hospital, Seoul, Korea; 2Division of Acute Care Surgery, Korea University Anam Hospital, Seoul, Korea; 3Division of Critical Care Medicine, Ewha Womans University Mokdong Hospital, Seoul, Korea; 4Department of Surgery, Yonsei University College of Medicine, Seoul, Korea; 5Division of Nephrology, Yonsei University College of Medicine, Seoul, Korea; 6Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea; 7Division of Nephrology, Korea University Anam Hospital, Seoul, Korea; 8Department of Surgery, Yonsei University College of Medicine, Seoul, Korea
Background: According to the current Center for Korean Network for Organ Sharing guidelines for kidney transplantation from brain-dead donors with hepatitis B or C infection, organs from HBsAg(+) or anti-HCV(+) donors can only be transplanted into HBsAg(+) or anti-HCV(+) recipients. We aimed to confirm the current status and kidney transplantation results from brain-dead donors with hepatitis B or C virus in Korea and to identify strategies for resolving donor-recipient disparity.
Methods: This retrospective study included all kidney transplantations from brain-dead donors in the Korean Organ Transplantation Registry database between January 2015 and June 2020, divided into three groups according to donor hepatitis status. Finally, kidney transplantations from 80 HBV(+), 12 HCV(+), and 2,013 HBV(-)/HCV(-) donors were included.
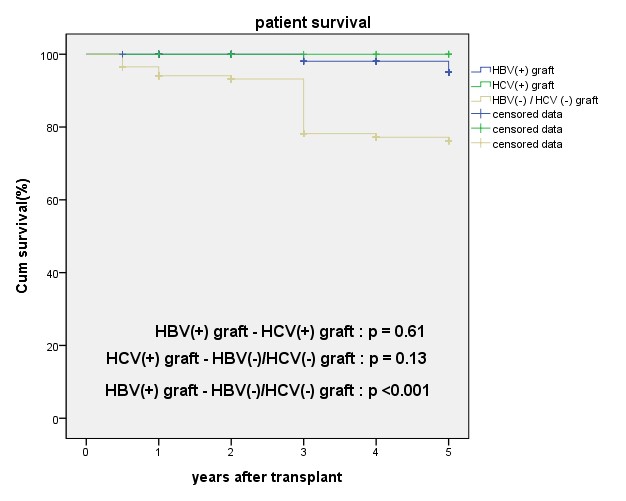
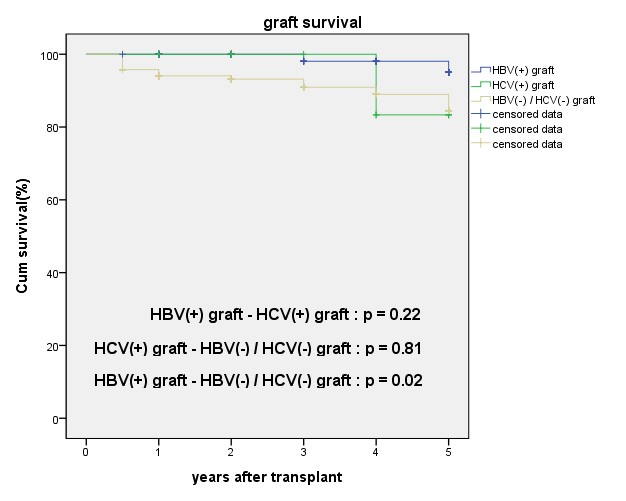
Results: No statistically significant differences were observed in the follow-up period, number of kidney transplants, postoperative hospital days, survival rate, serum creatinine from baseline to 5 years, cause of graft loss, complications, or rejection between the three groups. Five-year graft survival rates of the HBV(+), HCV(+), and HBV(-)/HCV(-) recipients were 95%, 83.3%, and 84.5%, respectively [HBV(+)-HCV(+), p = 0.22; HCV(+)-HBV(-)/HCV(-), p = 0.81; HBV(+)-HBV(-)/HCV(-), p = 0.02]. Five-year patient survival rates of the HBV(+), HCV(+), and HBV(-)/HCV(-) recipients were 95%, 100%, and 76.2%, respectively [HBV(+)-HCV(+), p = 0.61; HCV(+)-HBV(-)/HCV(-), p = 0.13; HBV(+)-HBV(-)/HCV(-), p < 0.001].
Conclusion: HBV(+)/HCV(+) brain-dead donor kidney transplantation outcomes were comparable to HBV(-)/HCV (-). Thus, South Korea can begin transplantation from HBV(+) or HCV(+) donors to HBV(-) or HCV(+) recipients as soon as possible, giving many patients hope.
This research was supported by the "National Institute of Health" research project (Project No.2014-ER6301-00, 2014-ER6301-01, 2014-ER6301-02, 2017-ER6301-00, 2017-ER6301-01, 2017-ER6301-02, 2020-ER7201-00) .
Lectures by Hanyoung Lee
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Thu-19 13:00 - 14:00 |
ECD / Living Donation | Kidney transplantation from brain-dead donors with hepatitis B or C in South Korea: a 2015–2020 korean organ transplantation registry data analysis | South Seas Ballroom A/B |
