A novice surgeon's perspective on pure laparoscopic donor right hepatectomy – a single-center study of the first 40 cases
Changho Seo1, Yoonyoung Choi2, Youngkyoung You2, Gunhyung Na1, Hojoong Choi2.
1Surgery, Bucheon St. Mary’s Hospital, The Catholic University of Korea, Seoul, Korea; 2Surgery, Seoul St. Mary’s Hospital, The Catholic University of Korea, Seoul, Korea
Introduction: While laparoscopic major hepatectomy has been increasing in popularity, PLDRH still requires careful consideration due to the need for donor safety and high-quality grafts. The role of novice surgeons in performing PLDRH is still controversial, and limited data are available on the outcomes of PLDRH performed by novice surgeons. Therefore, this study aims to evaluate the early outcomes of PLDRH performed by a novice surgeon in a single-center.
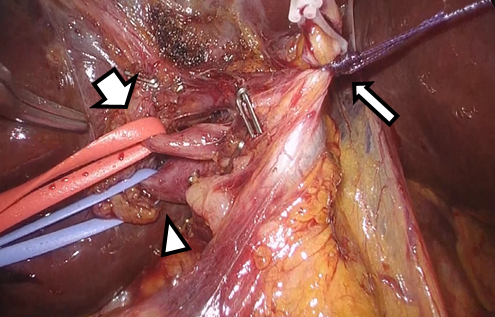
Method: From March 2019 to April 2021, a total of 86 patients underwent donor right hepatectomy at Seoul St. Mary's Hospital, of which 40 underwent PLDRH and 46 underwent open hepatectomy. A single surgeon with less than 10 years of experience in an independent position performed all operations during the study period. PLDRH was performed using a flexible scope and five ports. Initially, patients with anatomical variations were excluded, but the inclusion criteria were later expanded to include patients with anatomical variations using external traction of the cystic duct method.
Results: Their mean age was 37.5 ± 12.9 years and 20 (50.0%) were female. The average BMI was 23.3 and the average graft volume was 795.7 ml. The mean graft steatosis was 2.8%. There were 5 patients (12.5%) with portal vein variation, and 12 patients (30.0%) with duct variation. The average operation time was 321.5 minutes and the time from hepatic artery clamping to graft out was 18.4 minutes. There was no intraoperative transfusion and no open conversion in all patients. The average hospital stay was 10.5 days after surgery. There were two patients who have biliary complication, and one patient underwent re-operation due to wound bleeding. There were no statistically significant differences in baseline characteristics between the PLDRH and open groups, except for BMI. The operation time for the PLDRH group was significantly longer than that for the open group. There were no significant differences between the two groups in terms of complication rates, rates of biliary complications, or rates of reoperation.
Conclusion: PLDRH remains a challenging procedure that requires experience in both laparoscopic and open hepatectomy. The external traction of the cystic duct method may be helpful for junior surgeons performing PLDRH for the first time. The findings of this study could establish the safety and feasibility of PLDRH by novice surgeons and provide insights into the required training and supervision for this complex procedure.