
Why do only 2 out of 3 consented paediatric donors proceed to donation surgery?
Elena Cavazonni1,3, Lukas Staub2, Kiera Robinson2, Tali Klein3, Michael J O'Leary1.
1NSW Organ and Tissue Donation Service, Sydney, Australia; 2Talus Research Consulting, Manly, Australia; 3Pediatric Intensive Care Unit, Children’s Hospital Westmead, Sydney, Australia
Introduction: The Australian organ donation national reform was a successful initiative that saw an increase over ten years of actual deceased donors by 122% and an associated increase in transplantation rate of 81%. This increase in donations resulted from an iterative journey that established appropriate identification processes for all potential donors, embedded a collaborative family approach and engaged the transplant sector for the optimal use of all potential donor grafts. Disappointingly, this donation growth was not seen in the paediatric donor population.
Method: We aimed to assess the reasons for non-conversion in the paediatric donor population by utilising data from the Australian DonateLife life death audit. The audit collects real-time demographic of all hospital deaths in the ICU, ED and patients discharged from the ICU to the ward in the previous 24 hours. DonateLife staff audit 90 hospitals in Australia, and we obtained data for all paediatric deaths (age 0-15) from 1 January 2016 to 31 December 2021. As acceptance of paediatric organs is based on the donor's size, as such we used age as a surrogate for weight as the audit does not collect weight as a data point.
Results: During the period studied, there were 260 consented paediatric donors with 172
actual deceased paediatric donors, a conversion rate of 66%. Our results showed a linear relationship between the donor's age and conversion, with the youngest/smallest donors proceeding to donation 20% of the time and those greater than five years of age converting 87%. Pleasingly gender did not impact conversion, and as expected donation pathway revealed that only 38% of DCDD progressed to donation surgery compared to 90% via the DNDD pathway. The most common reasons for the lack of conversion were “no suitable recipient”, “not suitable to proceed”, “did not die in the timeframe for DCD”, and “failed physiological supports”. The not suitable to proceed and failed physiological support were not different when stratified by age. However, when we reviewed the “no suitable recipient”, this was reported predominantly in donors under two months of age.
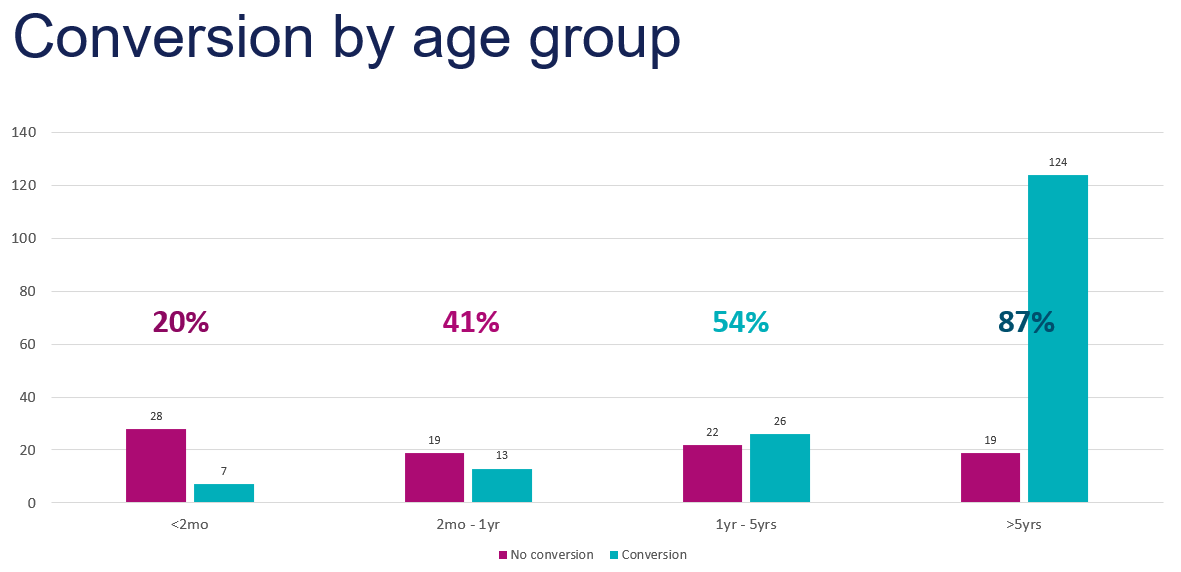
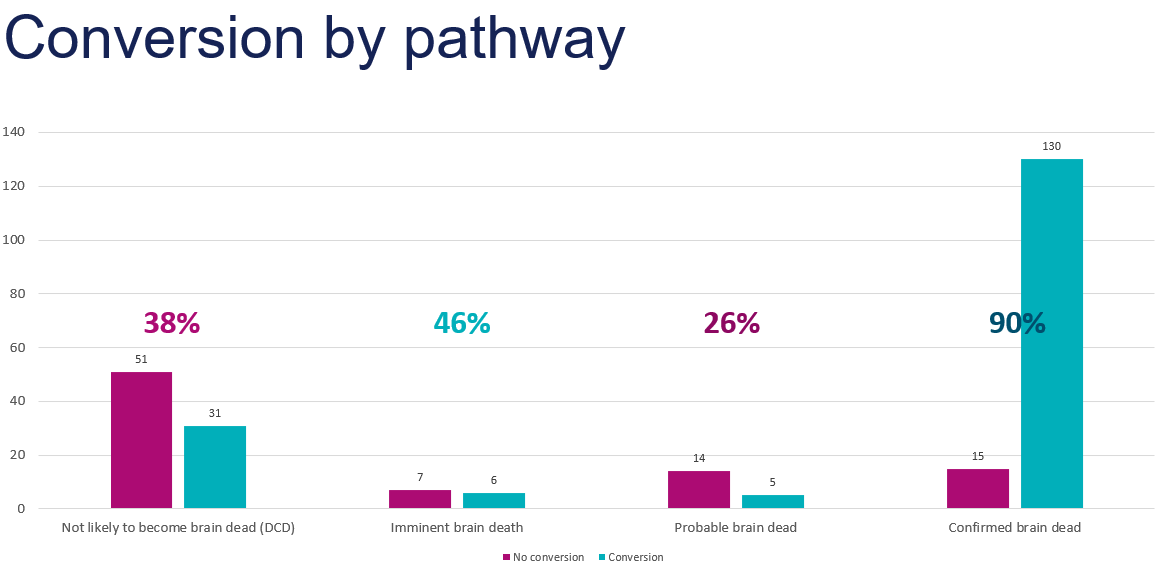
Conclusion: In summary, consented paediatric donors are less likely to proceed to donation surgery if they are a DCDD case and less than five years of age, and even more if they are less than two months of age. Therefore, the donation sector needs to work collaboratively with the transplant sector to see if we can optimise the utilisation of grafts from our youngest/ smallest donors. Furthermore, ICU education in donor management care and the establishment of a rapid retrieval process could help reduce the number of “failed physiological support” cases.