Tetsuya Tajima, United States has been granted the ISODP Congress Scientific Award
Dr. Tetsuya Tajima completed his 6-year surgery residency and joined the Division of Hepato-Biliary-Pancreatic Surgery and Transplantation at Kyoto University, Japan as a surgical instructor in 2016. The division started a liver transplantation program in 1990, and to date, it has performed more than 1,900 living-donor liver transplants, more than any other institution in Japan. Dr. Tajima has been involved in both basic and clinical research in liver transplantation. In 2021, Dr. Tajima obtained his Ph.D. and in 2022 an M.P.H. at Kyoto University, respectively.
Dr. Tajima joined Krams and Martinez Labs (Transplant Immunology Labs), at Stanford, as a Postdoctoral Scholar in April 2022 and was awarded an internal Transplant and Tissue Engineering Center of Excellence Fellowship for his studies examining refractory rejection after liver transplant in an experimental model. Dr. Tajima is working on the DoD-funded project where he is using high-dimensional mass cytometry (CyTOF) to discern the functional significance of specific myeloid and T cell populations during rejection in a mouse model of vascularized composite allotransplantation (VCA). In addition, Dr. Tajima is conducting clinical research on Epstein-Barr virus (EBV)-associated post-transplant lymphoproliferative disorders (PTLD), the impact of induction therapy on rejection in pediatric transplantation, and risk factors for EBV DNAemia in pediatric transplantation using data from a prospective multicenter study in the United States, which was supported by a grant from the National Institutes of Health. Dr. Tajima was the recipient of the Japan Society for Transplantation Award 2022, the IPTA (International Pediatric Transplant Association) Congress Scientific Award 2023 and will receive the Japanese Society of Hepato-Biliary-Pancreatic Surgery Presidential Award in 2023.
Risk factors for Epstein-Barr virus DNAemia in pediatric transplantation: A multicenter study in the United States
Tetsuya Tajima1, Daniel Bernstein2, Scott D Boyd3, Dita Gratzinger3, Grant Lum1, Kazunari Sasaki1, Brent Tan3, Kenneth Weinberg2, Brian Armstrong4, Meredith Brown5, Clifford Chin6, Dev Desai7, Thomas M Fishbein8, George Mazariegos9, Mark A Robien5, Akin Tekin10, Clare J Twist11, Robert S Venick12, Sheri M Krams1, Olivia M Martinez1, Carlos O Esquivel1.
1Department of Surgery, Division of Abdominal Transplantation, Stanford University School of Medicine, Stanford, CA, United States; 2Department of Pediatrics, Stanford University School of Medicine, Stanford, CA, United States; 3Department of Pathology, Stanford University School of Medicine, Stanford, CA, United States; 4Rho, Durham, NC, United States; 5National Institute of Allergy and Infectious Diseases, Rockville, MD, United States; 6Department of Pediatrics, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, United States; 7Division of Surgical Transplantation, UT Southwestern Medical Center, Dallas, TX, United States; 8Departments of Surgery and Pediatrics, MedStar Georgetown University Hospital, Washington, DC, United States; 9Department of Pediatrics, UPMC Children’s Hospital, Pittsburgh, PA, United States; 10Department of Surgery, University of Miami Miller School of Medicine, Miami, FL, United States; 11Department of Pediatric Oncology, Rosewell Park, Buffalo, NY, United States; 12Department of Pediatric Gastroenterology, David Geffen School of Medicine at UCLA, Los Angeles, CA, United States
Clinical Trials in Organ Transplantation in Children (CTOTC-06).
Introduction: Epstein-Barr virus (EBV) is associated with clinical symptoms, such as lymphadenopathy, fever, and hepatitis as well as development of EBV+ post-transplant lymphoproliferative disorders (PTLD), which is the most common malignancy in children after transplant; however, there is insufficient evidence of risk factors for EBV DNAemia investigated based on prospectively collected data in pediatric transplantation.
Methods: This prospective, multicenter, study (NCT02182986) enrolled 944 children (≤ 21 years of age). Of these, 872 patients received liver, heart, kidney, intestinal, or multivisceral transplants (LT, HT, KT, and IT, respectively) in seven US centers between 2014 and 2019 (NCT02182986). EBV DNAemia was monitored by collecting blood samples prospectively (n = 4753) at multiple timepoints: enrollment or transplant, every 3 months during the first 2 years, twice yearly thereafter. After patient selection, 470 patients (261 LTs, 97 HTs, 79 KTs, and 33 ITs) were retrospectively analyzed. The clinical variables included sex, age, race, ethnicity, pre-transplant EBV and cytomegalovirus (CMV) serologies, and induction therapy. Cumulative incidence of EBV DNAemia within a year of transplant was compared, with patient death as a competing risk.
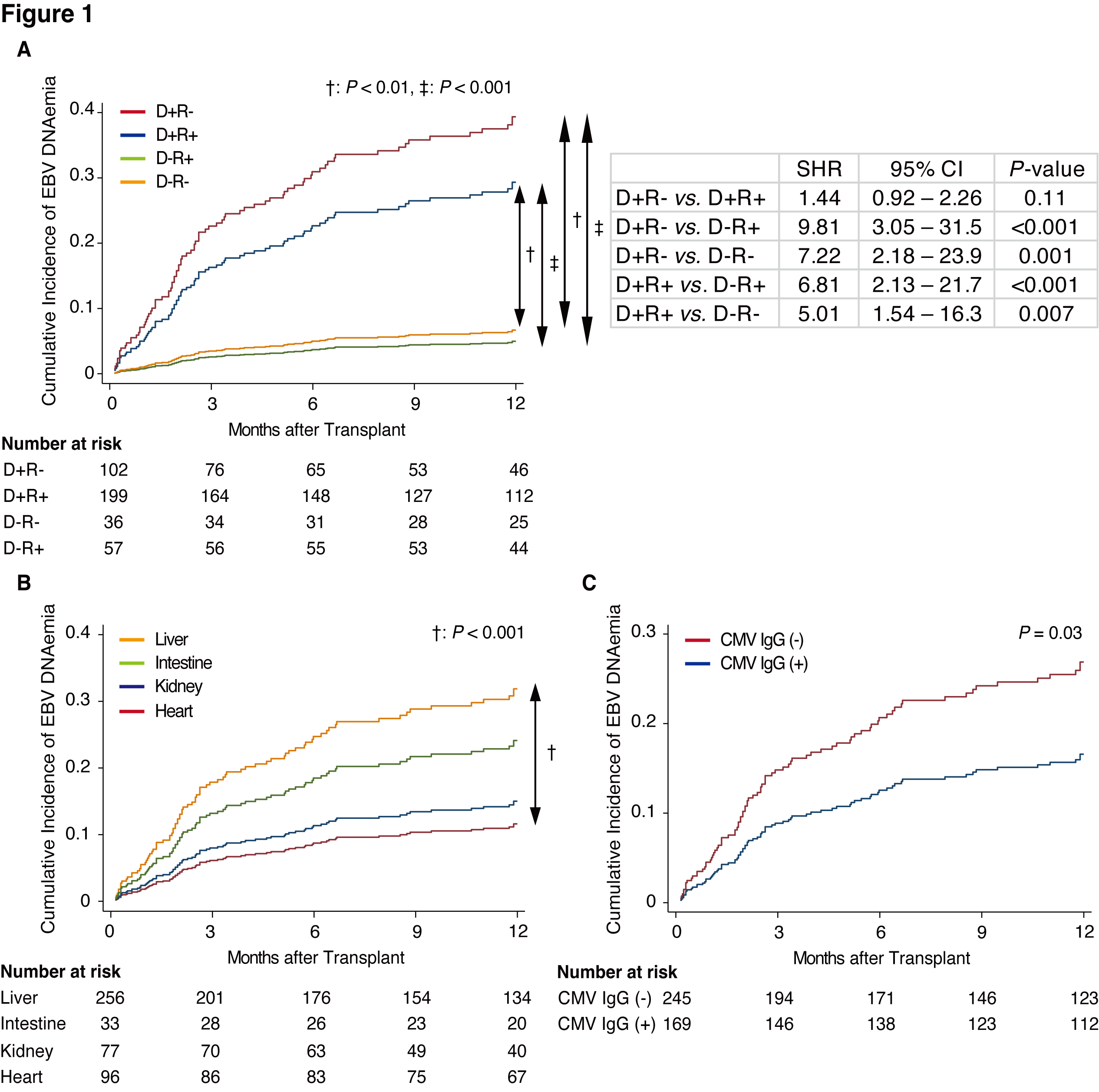
Results: The cohort included 265 males and 205 females, and the median age at transplant was 4.1 years (IQR: 1.3–12.7). Uni/multivariable analyses revealed the combination of EBV-seropositive donor and EBV-seronegative recipient (D+R-) vs. D-R+ (sub-hazard ratio: 9.81 [3.05–31.5], P <0.001), D+R- vs. D-R- (7.22 [2.18–23.9], P =0.001), D+R+ vs. D-R+ (6.81 [2.13–21.7], P <0.001), and D+R+ vs. D-R- (5.01 [1.54–16.3], P =0.007) were significant risk factors for EBV DNAemia within a year post-transplant (Fig. 1A). Additionally, LT vs. HT (3.11 [1.54–6.28], P =0.002) and CMV IgG-negative recipient (1.73 [1.05–2.85], P =0.03) were also significant risk factors for EBV DNAemia within a year post-transplant (Fig. 1B, 1C)
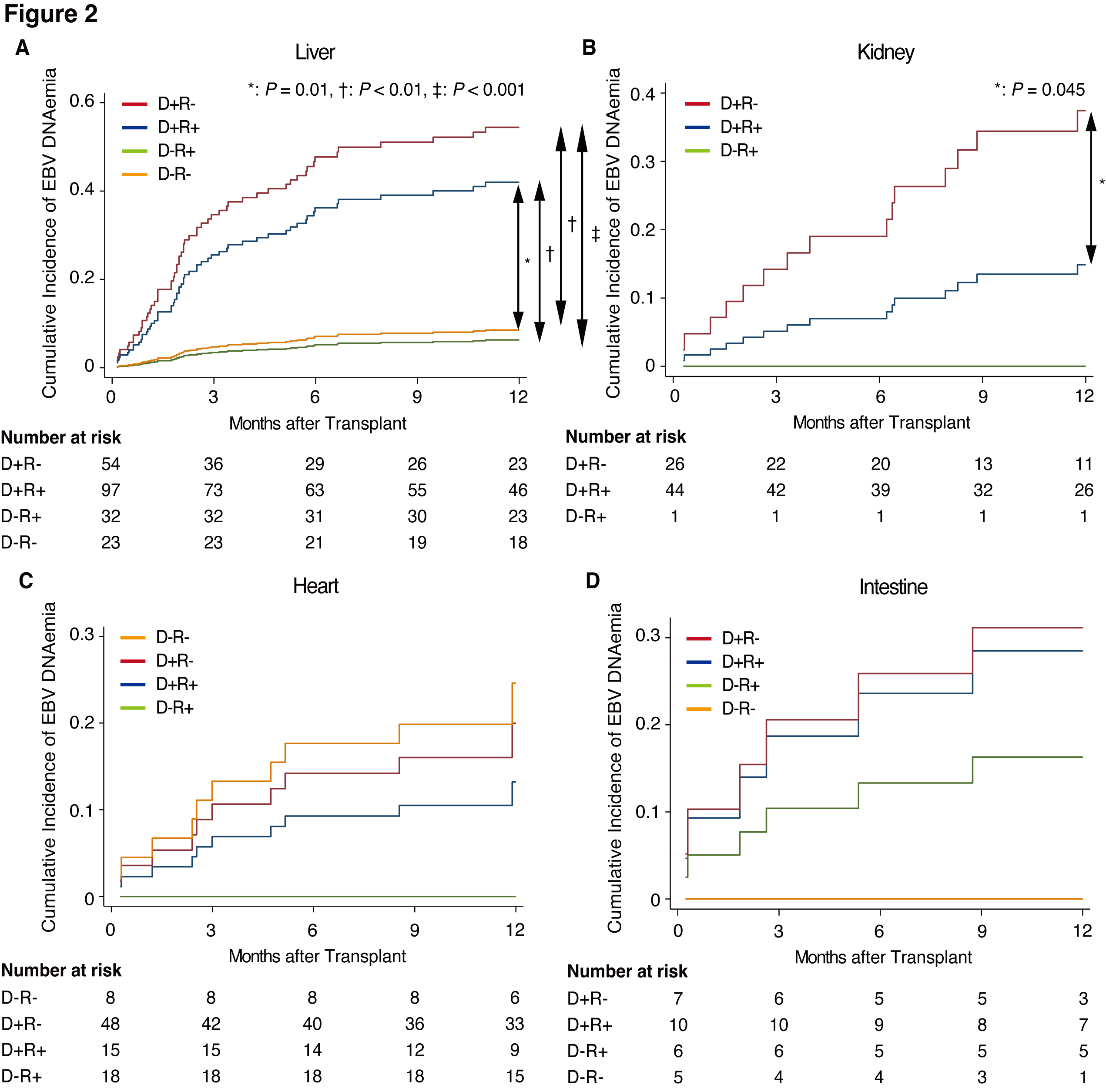
Subgroup analyses for each transplanted organ showed that D+R-, D+R+, and CMV-IgG+ in LT, younger age in KT, and CMV-IgG+ in HT were significant risk factors for EBV DNAemia. Focusing on D/R relationship, LT showed a similar impact of D/R relationship on EBV DNAemia to the entire cohort (Fig. 2A). In contrast, KT presented a significantly higher incidence rate of EBV DNAemia in D+R- than in D+R+ (Fig. 2B). HT and IT showed almost similar incidences of EBV DNAemia in all groups except D-R+ and D-R- groups, respectively (Fig. 2C, 2D).
Conclusions: Of note, D+R- as well as D+R+ were risk factors for EBV DNAemia compared to the D- group, suggesting that EBV-seropositive recipients were probably reinfected by genetically different EBV from recipients’ EBV. The fact that D+R+ patients, the most common population of transplant recipients, are more likely to develop EBV DNAemia than recipients of EBV-naïve organs should be emphasized in terms of post-transplant follow-up.
This study was funded by NIH UO1 AI104342, UM2AI117870 (Rho Federal Systems), and the Stanford Transplant and Tissue Engineering Center of Excellence fellowship..