Systematic reporting and investigation of possible infection of donor origin as part of best practice in transplantation
Ines Ushiro-Lumb1, Olive McGowan1, Jeanette Foley1, Derek Manas1, Richard Baker1.
1Organ & Tissue Donation and Transplantation, NHS Blood and Transplant, London, United Kingdom
Introduction: In the UK, post-transplant events that may have an impact on allograft recipients must be centrally reported to the Organ and Tissue Donation and Transplantation service. This should be done as soon as an event which could be donor-related is recognised, and reporting should not be delayed whilst awaiting confirmation. Notification triggers prompt dissemination of information to transplant centres and initiates a systematic investigation. A report with findings, actions, and recommendations is essential; co-operation from all stake holders and a multi-disciplinary approach are key to improved practice and better patient outcomes.
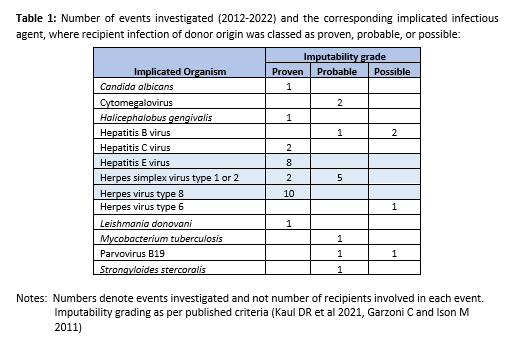
Methods: A review of the outcome of extensive investigations over a period of 10 years, where donor-derived transmission of infection was concluded to have been possible, probable, or proven was performed. General biovigilance principles of serious adverse event investigation applies to all cases. The specific methods used to confirm or refute infection of donor origin vary depending on the pathogen involved.
Results: During this period 14,949 donors enabled 38,380 organ transplants, with an observed 0.3% rate of donor-related transmission of infection events per proceeding donor. This is based on events that have become known and were investigated; under-reporting is likely to have occurred. The agents most commonly implicated were Human Herpes Viruses, mainly herpesvirus type 1,2, and 8, followed by Hepatitis E Virus (see table 1); of note, herpesvirus type 8 alone was responsible for a quarter of all cases and was the most frequent imputable pathogen. Cases where the donor was excluded as possible source of infection in the recipient, or where imputability could not be ascertained, are not included in this summary.
Conclusions: Unintended transmission of infection of donor origin is infrequently demonstrated but it may be associated with significant recipient morbidity and mortality. Patient and public perception of safety of transplantation may also be negatively impacted by such events. Transmission patterns cannot be applied universally as these will depend on specific local circumstances such as prevalence of infection, amongst many other factors. It is nevertheless essential that all those involved in organ donation and transplantation remain attentive to potential occurrences, so that they can be detected, notified, and appropriately managed. Critical analysis of these events is important for the identification of possible deficiencies, need for change and learning. This also has the potential to improve organ utilisation in a safe manner, by enabling the implementation of appropriate preventative or mitigating measures that can decrease the level of risk to recipients. In our setting, this process is continuously used to inform best practice.