Preventable harm in the Canadian organ donation and transplantation system (semi colon) a descriptive study of missed organ donor identification and referral
Samara Zavalkoff1, Sam Shemie1,2, Jehan Lalani2, Shauna O'Donnell1, Lee James2, Isabella F Karam1.
1Pediatric Intensive Care Unit, McGill University Health Centre, Montreal, QC, Canada; 2System Development, Organ Donation and Transplantation, Canadian Blood Services, Ottawa, ON, Canada
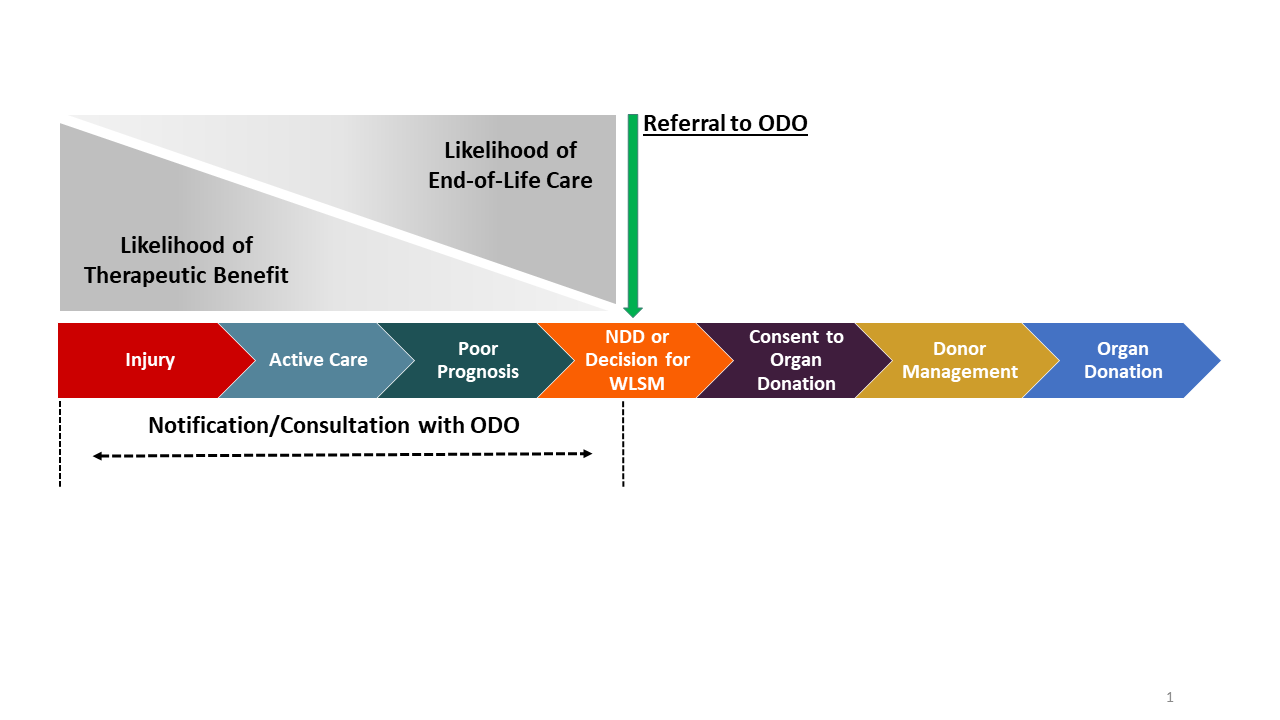
Introduction: Deceased organ donation is predicated on timely identification and referral (IDR) of potential organ donors, as failure to perform this first, critical step jeopardizes the downstream donation process (Figure). Many Canadian provinces have legislated mandatory referral of potential deceased donors; yet, untimely or missed IDR are examples of missed donation opportunities (MDO) which are safety events where best or expected practice has not occurred. MDOs cause preventable harm to patients and families denied the opportunity of donation at end of life (EOL), and transplant waitlist patients denied access to lifesaving organs.
Currently the Canadian organ donation and transplantation (ODT) system is unable to quantify this preventable harm, nor plan and monitor improvement initiatives to reduce it. Our objective was to determine the national rate of donor IDR, estimate the number of MDO from missed IDR, and quantify the consequential preventable harm to Canadians patients and their families at the EOL and on the transplant waitlist.
Figure
Method: We requested donor definitions and data to calculate IDR, consent, and approach rates from all 11 Canadian organ donation organizations (ODO) for 2016–2018. We then estimated the number of missed IDR patients who were eligible for approach (safety events) and the associated preventable harm to patients at EOL and on transplant waitlists.
Results: Annually, there were 63–76 missed IDR patients eligible for approach (3.6–4.5 per million population [PMP]) from four ODO — three with mandatory referral legislation. Applying each ODO’s approach and consent rates for the corresponding year, there were 37–41 missed donors (2.4 donor PMP) annually. Assuming three transplants per donor, the theoretical number of missed transplants would be 111–123 (6.4–7.3 transplants PMP) annually.
Data from the four Canadian ODO demonstrates that missed IDR safety events resulted in important preventable harm measured by a lost opportunity for donation of 2.4 donors PMP annually and 354 potentially missed transplants between 2016–2018.
Conclusion: Missed identification and referral of potential organ donors causes harm by denying both the opportunity to donate at end of life and access to lifesaving or life-enhancing organs to vulnerable patients awaiting transplant. This safety event and its consequential preventable harm is unmeasured and unrecognized, so there is no accountability or disclosure of these patient safety events. Future work is needed to standardize the definition of a potential donor, clinical referral triggers, and the reporting of missed donor identification and referral to allow for accurate measurement and reporting of these patient safety events and to facilitate accountability mechanisms.