Organ procurement failure in a tertiary government hospital in the Philippines: why are we losing our potential donors?
Delbrynth M Smigel1, Julie Ann Kristy L Torres2, Shafiq Dexter B Abou Zaki2, Fiona Therese Beldua3, Ayla Angelica Carreon-Ysulat3, Giannina Krishna Go-Ong2, Maria Theresa L Bad-ang3.
1Division of Trauma and Surgical Critical Care, Department of Surgery, Southern Philippines Medical Center, Davao City, Philippines; 2Section of Neurology, Department of Internal Medicine, Southern Philippines Medical Center, Davao City, Philippines; 3Section of Nephrology, Department of Internal Medicine, Southern Philippines Medical Center, Davao City, Philippines
Background: Deceased donor organ donation in the Philippines remains to be one of the lowest in the world. Differences in religion, ethnicity, education, unavailability of proper equipment and trained personnel for organ retrieval, and lack of government support are few of the factors that have contributed to the steady decline of organ donors in the country. The purpose of this study was to describe the causes of organ procurement failure in our setting.
Methods: A retrospective review of the charts of potential donors listed in the Southern Philippines Medical Center (SPMC) Human Advocate Retrieval Effort (SHARE) database from February 1, 2022 to April 12, 2023 was done. Demographics, clinical characteristics, and procurement information were collected. The causes of non-eligibility of potential donors, as well as failure of organ procurement for eligible donors were identified.
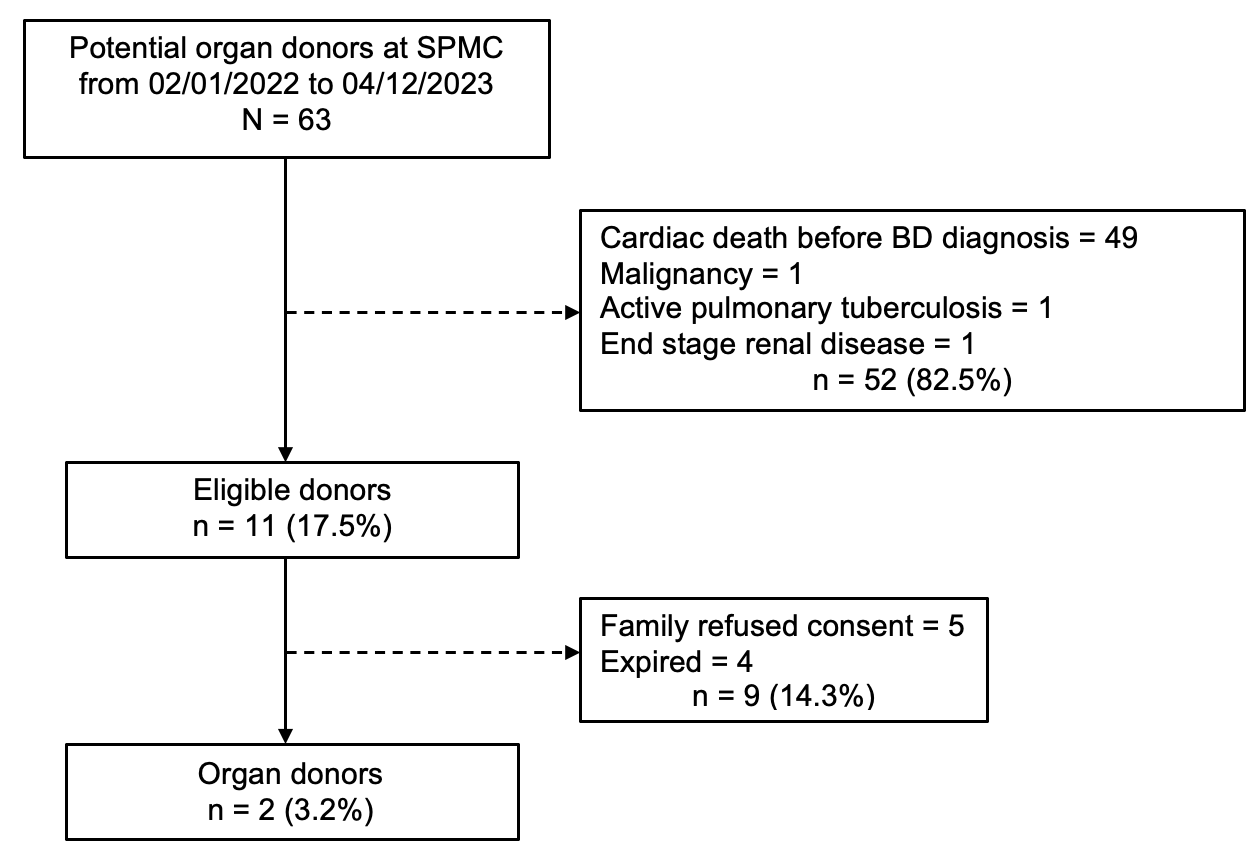
Results: For the 14-month study duration, there were 63 potential donors referred to the SHARE Team. The median age of the patients was 46 years, 42 (66.7%) were males, 61 (96.8%) were Christians, and 2 (3.2%) were Muslims. 30 (47.6%) patients were admitted due to Trauma while 33 (52.4%) were non-Trauma cases. There were only 11 (17.5%) patients who were eligible. Non-eligibility were mainly due cardiac death prior to brain death (BD) diagnosis (77.8%), with some cases of malignancy (1.6%), active pulmonary tuberculosis (1.6%), and progression to end-stage renal disease (1.6%). Of the eligible patients, family refusal (7.9%) and death prior to organ procurement (6.3%) were the causes for procurement failure. There were only 2 (3.2%) patients who donated, all of which were eye tissues only.
Conclusion: We identified that our institution needs a lot of work in maintaining our potential donors long enough until BD diagnosis, as well as our eligible donors until organ procurement. While there is a limitation in equipment, infrastructure, and manpower in our setting, these identified causes must be addressed urgently to increase our procurement rate.