Intestinal grafts from paediatric donors after circulatory death
Eva Flores Cabeza1, Belén Estébanez Montiel1, Carmen Gómez Aragón1, Ane Miren Andrés Moreno2, Angel Aroca Peinado4, Alvaro González Rocafort4, Juvenal Rey Lois4, Pablo Millán Estañ1, Lucia Cachafeiro Fuciños1, Ana Moreno Núñez1, Cristina Rodríguez Pèrez1, Paula Burgos Morales4, Esther Ramos Boluda3, Belen Calderon LLopis6, Aida Alcolea Sánchez3, Mateo Bernardo Cobertera1, Francisco del Rio Gallegos5, Alonso Mateos Rodríguez5, Francisco Hernández Oliveros2.
1Transpantation Coordination Unit, Hospital Universitario La Paz, Madrid, Spain; 2Paediatric Surgery department, Hospital Universitario La Paz, Madrid, Spain; 3 Paediatric Gastroenterology department, Hospital Universitario La Paz, Madrid, Spain; 4Paediatric Cardiac Surgery department, Hospital Universitario La Paz, Madrid, Spain; 5Regional Transplant Coordination, Servicio Madrileño de Salud, Madrid, Spain; 6Paediatric Intensive Care Unit, Hospital Universitario La Paz, Madrid, Spain
Introduction: The use of donors after circulatory death (DCD) has increased in recent years, specially after the use of normothermic regional perfusion (NRP) for all solid organs except the intestines, mainly due to its susceptibility to broader ischemic damage.
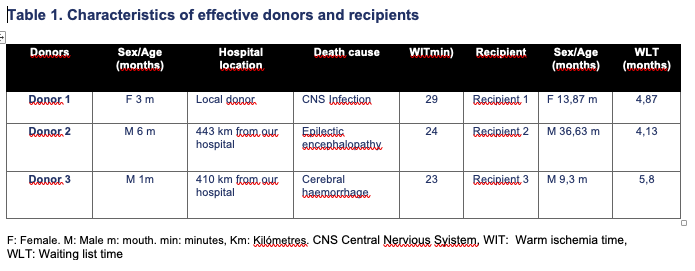
Method and results: Our team evaluated five multivisceral grafts from five potential pediatric DCD donors. Multivisceral grafts include intestines and, at least, two abdominal organs. In one case, the patient didn´t die at a time compatible with the donation. In another case, without heart recovery, the multivisceral graft was dismissed due to its appearance. The three remaining cases were actual organ donors, whose characteristics are shown in Table 1.
After making the decision to withdraw life support (LS), the possibility of donation was offered to the family. The patients were transferred to the operating room where, once everything had been prepared (surgical instruments, sterile field and ECMO (extracorporeal membrane oxygenation), the surgical team left the operating room. After that, the parents entered through a different door. Once the family had made their peace, intravenous heparin (3 mg/kg) was administered before the extubation. After withdrawing LS, significant hypoperfusion began. This happens when the mean arterial pressure is lower than 30mmHg in patients <1 year old, which is the case in all of our three patients. When the circulatory arrest happened, we asked gently for the parents to leave. Later, the surgical team went into the operating room using another door. According to spanish law, after five minutes, the death is confirmed. Simultaneous sternotomy and ligation of the supra-aortic trunks and cannulation of the infrarenal aorta and cava vein were performed. Following cannulation, NRP was started (the target flow is 2.6 L/min/m 2 ). The mean warm ischemia time (WIT) was 25,33 min (range 23-29). The heart spontaneously began to beat after starting ECMO without the need for defibrillation, at a mean time of 1,33 minutes (range 1-2 min). The patients were reintubated and vasopressor support was started. The multivisceral grafts presented good perfusion. In this situation, the ECMO flow was decreased progressively until withdrawal 23,33 min later. The procurement was similar to that of brain death donors. Multivisceral grafts were implanted without any incident in recipients with intestinal failure and liver disease. Two recipients were discharged from the hospital. The most recent transplant recipient died two weeks after the transplant.
Conclusion: DCD is a possible source of organ donation also in the case of multivisceral grafts.