Estimating the donor potential in Germany: Systematic evaluation of all in-hospital deaths of patients with primary or secondary brain damage
Axel Rahmel1, Josephine Wadewitz1, Ana Paula Barreiros2, Christopher Nieß1.
1Deutsche Stiftung Organtransplantation - German OPO, Frankfurt / Main, Germany; 2Deutsche Stiftung Organtransplantation - German OPO, Mainz, Germany
Introduction: Organ donation rates in Germany are low in comparison to most other European countries. In order to get a better understanding of the underlying causes and the actual donor potential, a systematic evaluation of all in-hospital deaths of patients with primary or secondary brain damage (psBD) is mandatory since 2019. We present the analysis of first three years.
Method: Using a national standardized data set all patients that died during the hospital stay and had an ICD-code of a diagnosis linked to psBD were identified and thereafter further classified by an in-house coordinator supported by a coordinator of the German organ procurement organization (DSO) on request. More than 95% of all hospitals reported the DSO.
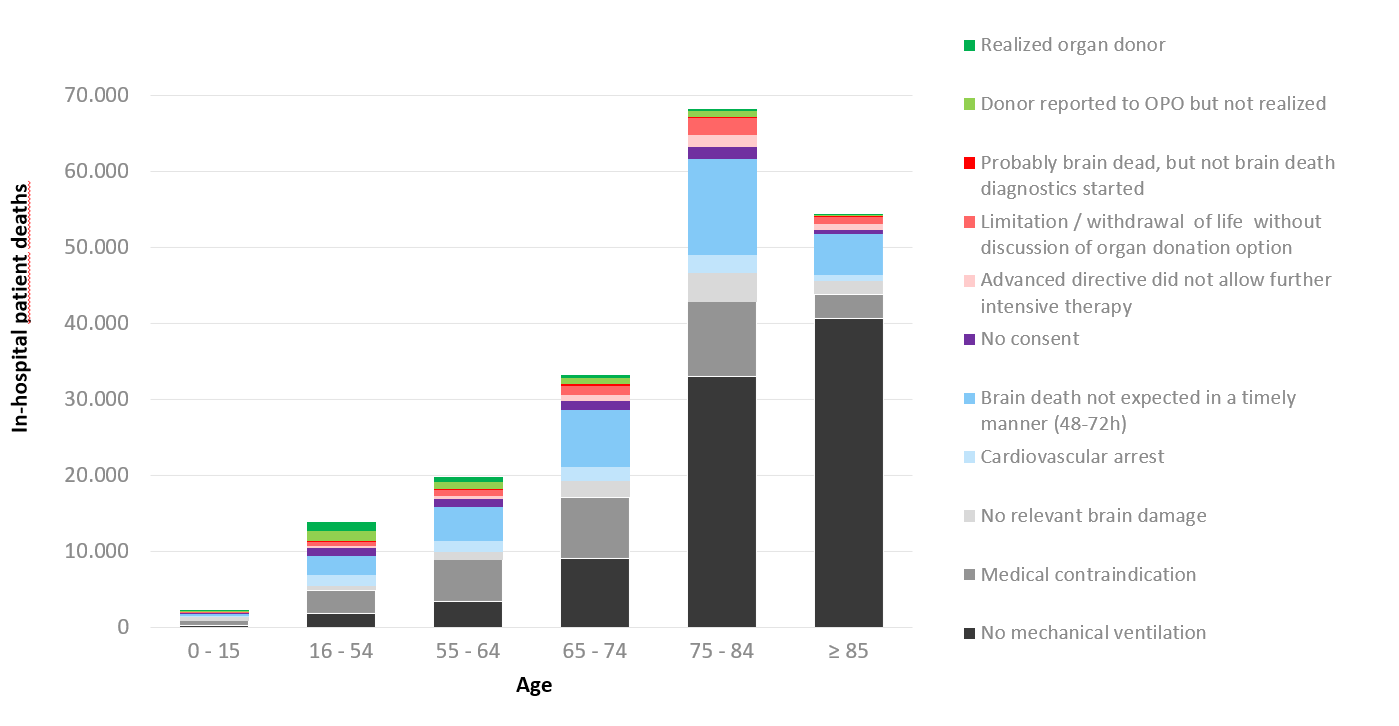
Results: From 2019-2021 a total of 191.775 patients (pts.) died with psBD in one of the 1190 donor hospitals in Germany. Of these, 88.358 (46%) were never put on mechanical ventilation, the vast majority being older than 75 years; 30.353 pts. (16%) showed a medical contraindication to organ donation; 9.670 pts. (5,0%) had no relevant psBD; 8.072 (4,2%) died of cardiovascular arrest in spite of optimal medical treatment; in 32.709 pts. (17,1%) brain death was not expected to occur (at all or at least in a time frame of 48-72 hours); of 5.742 pts (3,0%) objection to organ donation was known; in 3,700 an advanced directive prohibited further intensive care; intensive care was limited or withdrawn in 5.730 pts. (3,0%) cases without prior discussing the option of organ donation and 593 pts. were in retrospect probably already brain dead, but the necessary diagnostics to ascertain brain death were not initiated. 6.848 possible donors (3,6%) were reported to the DSO; 2.776 (1.4%) finally became organ donors. Figure 1 shows the different described categories by patient age.
Conclusion: This analysis shows that the number of organ donors after brain death could be increased by evaluating the option for organ donation prior to limiting or withdrawing life sustaining therapy and by initiating brain death diagnosis whenever indicated. In addition, intensive care to facilitate organ donation (ICOD) could further increase the donor potential. Most of these additional donors would probably be older than 65 years, though. Looking at the high number of patients where brain death was not expected to occur but that died of other causes, it seems plausible that the number of organ donors cold be substantially increased, if organ donation after circulatory determination of death would be established in Germany.