Expanding the boundaries of functional warm ischemia time (fWIT): successful kidney transplantation using normothermic machine perfusion (nmp) of a discarded kidney from uncontrolled circulatory determination of death donor
Devprakash Choudhary1, Sarbpreet Singh1, Shivkumar SP1, Arun Panjathia1, Vanji Nathan Subramani1, Amit Sharma1, Prof Deepesh B Kenwar1, Prof Ranjana Walker Minz2, Prof Ritambhra Nada3, Prof Sujata Wangkheimayum 4, Prof Harbir Singh Kohli5, Prof Ashish Sharma1.
1Department of Renal Transplant Surgery , PGIMER, Chandigarh , India; 2Department of Immunopathology , PGIMER , Chandigarh, India; 3Department of Pathology, PGIMER, Chandigarh, India; 4Department of Biochemistry, PGIMER, Chandigarh, India; 5Department of Nephrology, PGIMER, Chandigarh, India
Introduction: The global kidney shortage led to increased utilization of kidneys from donation after circulatory determination of death donors (DCD). However, a cut-off of 2-4 hours of warm ischemic time or functional warm ischemia time (fWIT-time from systolic blood pressure <50 mm Hg to cold organ flush, ideally less than 30 min-1hour) is used to exclude kidney donation at centres practising DCD transplantation. Unfortunately, more than 40% of DCD donors do not advance to donate due to prolonged time to death, representing potentially missed transplantation opportunities. Normothermic machine perfusion (NMP) has successfully utilized discarded livers and kidneys. In addition to reducing cold ischemia-induced injury, NMP restores viable organ function and provides objective evidence for organ viability assessment. However, the application of NMP on uncontrolled DCD(uDCD) kidneys is still a relatively unexplored area.
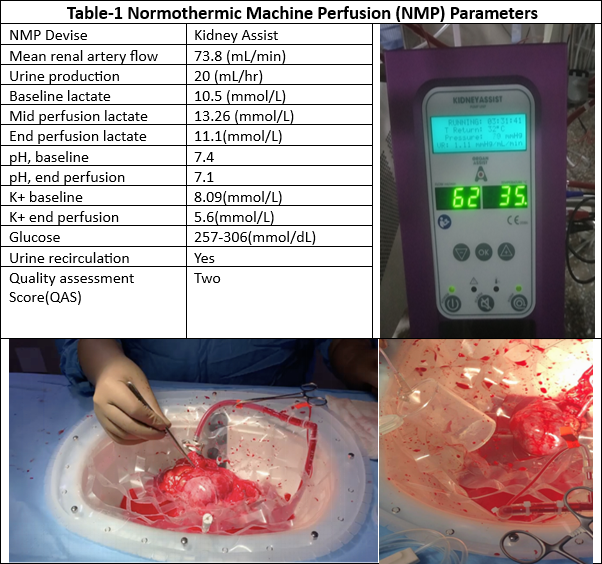
Methods: This report details the successful transplantation of a discarded kidney due to fWIT of 7 hrs from a 23-year-male donor with acute kidney injury (serum creatinine sCr-5.06 mg/dL). The donor was on triple inotropic support at retrieval and had nil urine output in the last four hours before uDCD. Upon retrieval, the left kidney underwent a successful back table cold flush, and after a cold ischemia time of 10h 24 min, the kidney underwent NMP for over three hrs on the Kidney AssistTM using study centres' red-cell based oxygenated perfusate. Kidney displayed multiple signs of viability (good macroscopic appearance), steady increase in renal blood flow(RBF), recorded a Quality assessment score of two (global pink appearance 1+ 0 for RBF > 50mll/hr + 1 for urine output <43ml/hr) and was transplanted in a 41-yr male. (Table-1)
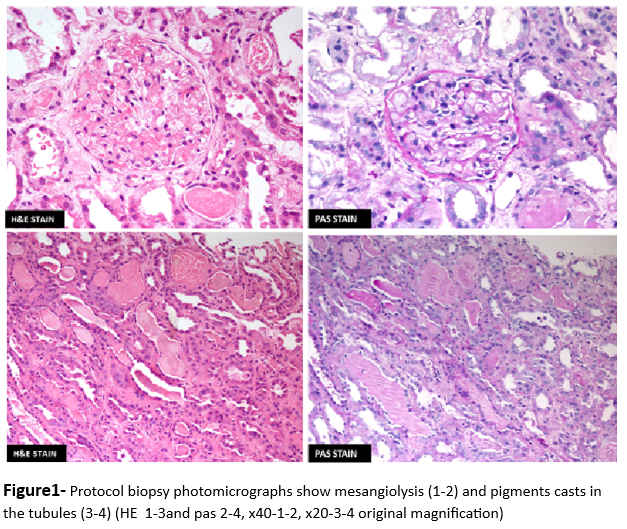
Results: The recipient experienced delayed graft function necessitating two weeks of hemodialysis. Protocol biopsy revealed severe acute tubular injury with cast nephropathy (Figure-1), showing no signs of rejection. The recipient was discharged after three weeks of inpatient care, and a baseline sCr of 1.2 mg/dl was achieved at three months post-transplant and remained 1-1.2 mg/dl throughout the subsequent 2yr follow-up period demonstrating the long-term success of the transplant.
Conclusion: The application of NMP for pre-transplant assessment and revitalization offers a novel method to validate the usability of kidneys, which are typically classified as unfit for transplantation. This is especially pertinent for kidneys from both DCD and uDCD donors that exhibit prolonged WIT and fWIT. Given the limitations set by WIT and fWIT cut-off times, implementing NMP could significantly expand the pool of transplantable kidneys, thereby facilitating a substantial increase in successful kidney transplantations.
Received Funding from PGIMER Chandigarh.