A model to estimate the impact of hospital length of admission on the residual risk of blood-borne virus infection in deceased organ donors
Martin Dutch1,2, Jonathan White3, Jonathan C Knott1,2.
1Department of Emergency Medicine, Royal Melbourne Hospital, Parkville, Australia; 2Department of Critical Care, University of Melbourne, Parkville, Australia; 3Faculty of Business and Economics, University of Melbourne, Parkville, Australia
Introduction: When potential organ donors undergo NAT testing for Blood borne infections such as hepatitis B (HBV), Hepatitis C (HCV) and Human Immunodeficiency Viruses (HIV), there remains a residual risk of undetected infection that has been acquired during the screening assay’s window period.
Current methods to estimate the residual risk of the patient having an infection at the time of blood draw have assumed that risk is homogenously acquired throughout the entire window period. For deceased organ donors, a proportion of these window periods are spent in hospital. For Australian organ donors, the risk of nosocomially acquired infection approaches zero.
Early viral infections are assumed to follow an exponential growth curve. The viral load at blood draw will vary based on the time of exposure. The ability of an assay to detect an infection follows a sigmoidal sensitivity curve as the viral load rises.
This study will model this sigmoidal relationship to estimate the attenuating impact of hospital length of stay on the residual risk of unexpected blood-borne virus transmission at the time of blood draw.
Methods: Our model is based on the current triplex assay used to screen deceased organ donors in Australia (Procleix® Ultrio Elite® Assay Grifols Diagnostic Solutions Inc. California, USA).
We estimate viral load at time of blood draw based on known viral doubling rates and an initial infective dose of 1 virion per 20mls. Manufacturer specified X50 & X95 detection limits were utilised. Assay sensitivity was assumed to follow the cumulative distribution function of the log normal distribution, with mean and variances inferred from the X50 and X95 calculations. The risk of acquiring infection, whilst in hospital, was assumed to approximate zero. Cumulative probabilities were summed over the event space, to calculate the overall residual risk.
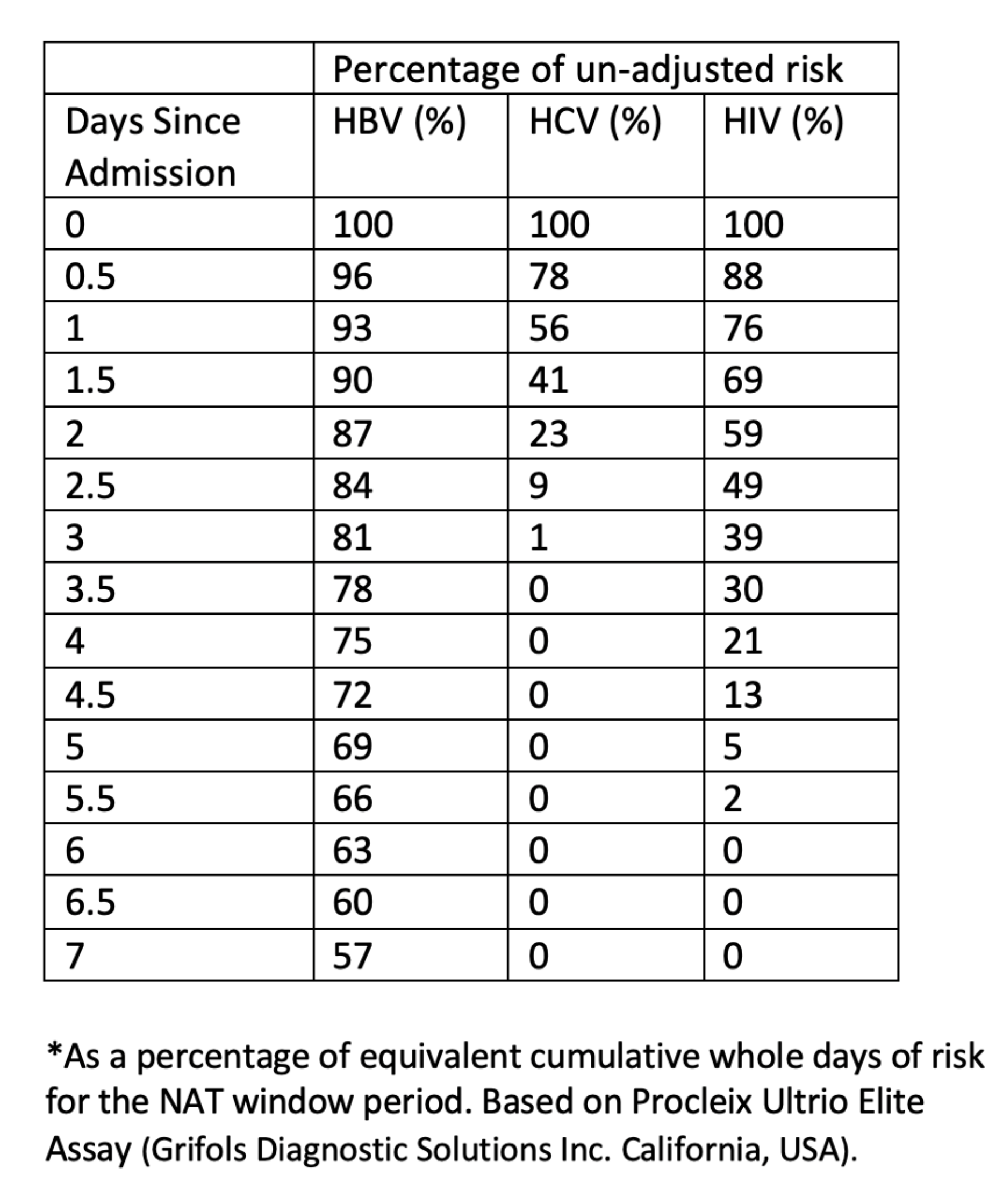
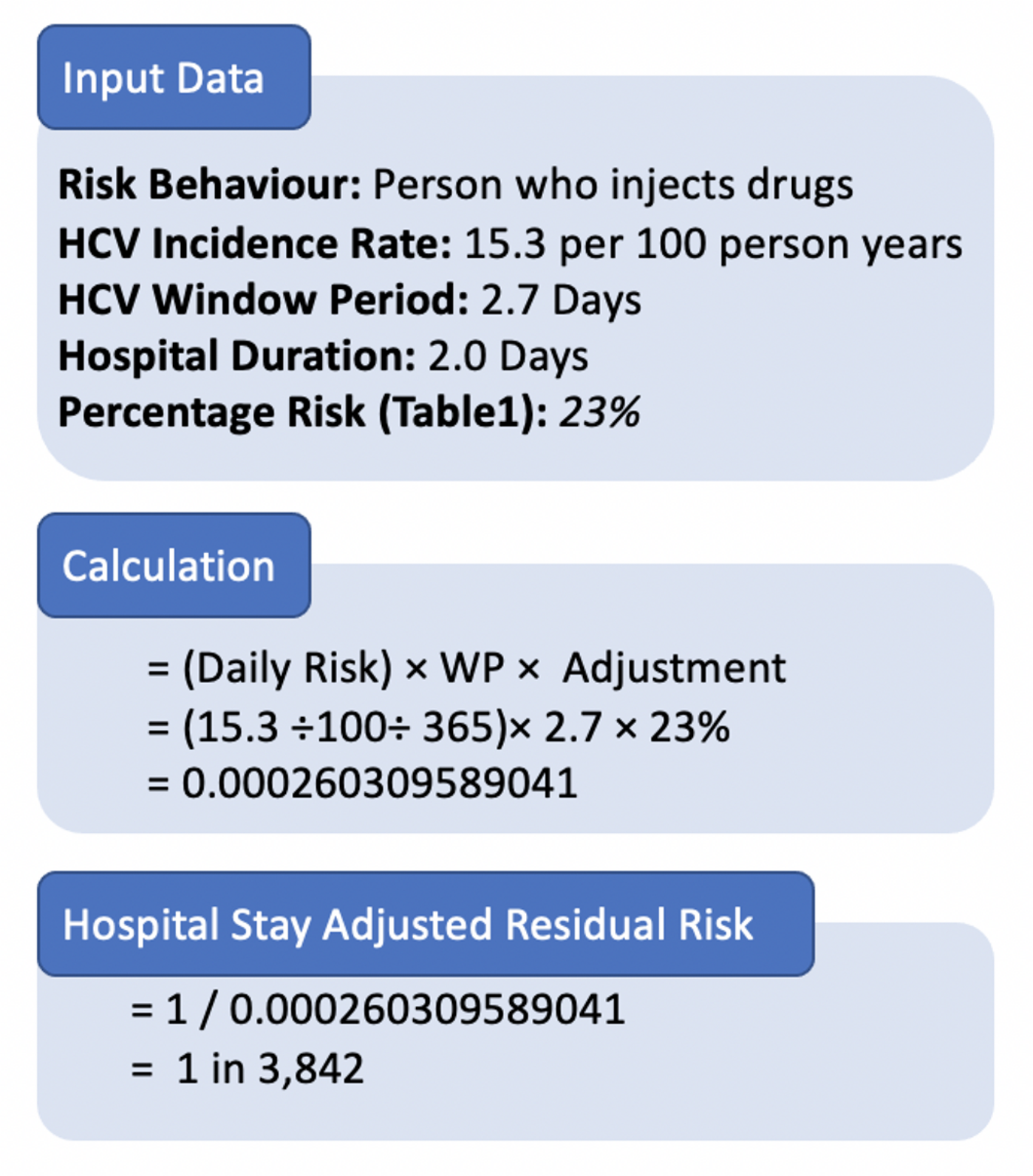
Results: The generated model demonstrates that residual risk reduces with the increasing length of admission for all viruses, showing a ‘hockey stick’ distribution of attenuation. Attenuation shows a 1:1 relationship for the majority of the window period. Approximately 7.9%, 4.9%, and 5.4% of the total cumulative risk are acquired outside the X50 LOD-derived window period. Hospital admission length of stay risk reduction is summarised in Table 1. Figure 1 demonstrates the calculation of the hospital admission length-adjusted residual risk for a given increased risk cohort.
Conclusion: This work provides a model for estimating the impact of hospital admission on the residual risks of blood-borne viruses. Hospital admission may significantly reduce the residual risk of infection, particularly where it approaches or exceeds the window period. The model may have utility in considering individual organ offers from increased viral risk donors.