
Examining the potential for uncontrolled organ donation subsequent to out-of-hospital cardiac arrest in Canada
Chelsea Lanos1,5, Alan M Batt2, Ian Drennan3, Sonny Dhanani4, Christian Vaillancourt5, Steve Lin6, Karim Solimon7, Dominique Cook1.
1Cardiff University, Wales, United Kingdom; 2Monash University, Victoria, Australia; 3Sunnybrook Hospital, Toronto, ON, Canada; 4The Children’s Hospital of Eastern Ontario, Ottawa, ON, Canada; 5Emergency Medicine, The Ottawa Hospital Research Institute, Ottawa, ON, Canada; 6St-Michaels Hospital, Toronto, ON, Canada; 7Lakeridge Health, Toronto, ON, Canada
Introduction: The demand for organs exceeds the amount of available organs through conventional organ donation pathways around the world. This has led to the exploration of alternative pathways, including the use of patients who have unsuccessful resuscitation subsequent to out-of-hospital cardiac arrest (OHCA). However there are no Uncontrolled Donation after Cardiac Death (uDCD) pathways that consider or utilize the OHCA population to address these shortages in Canada. Approximately 4,500 Canadians are on organ transplant waitlists at one time, with donation rates between 8.8 and 21.2 donors per million. There are an estimated 40,000 OHCAs each year in Canada, and a large majority are not transported by paramedics or do not survive, leaving behind a considerable population of potential donors eligible for uDCD. A critical review of the literature suggests that uDCD subsequent to OHCA is a viable opportunity to increase the organ donor pool in Canada, and quantifying this potential will inform future opportunities to increase donation.
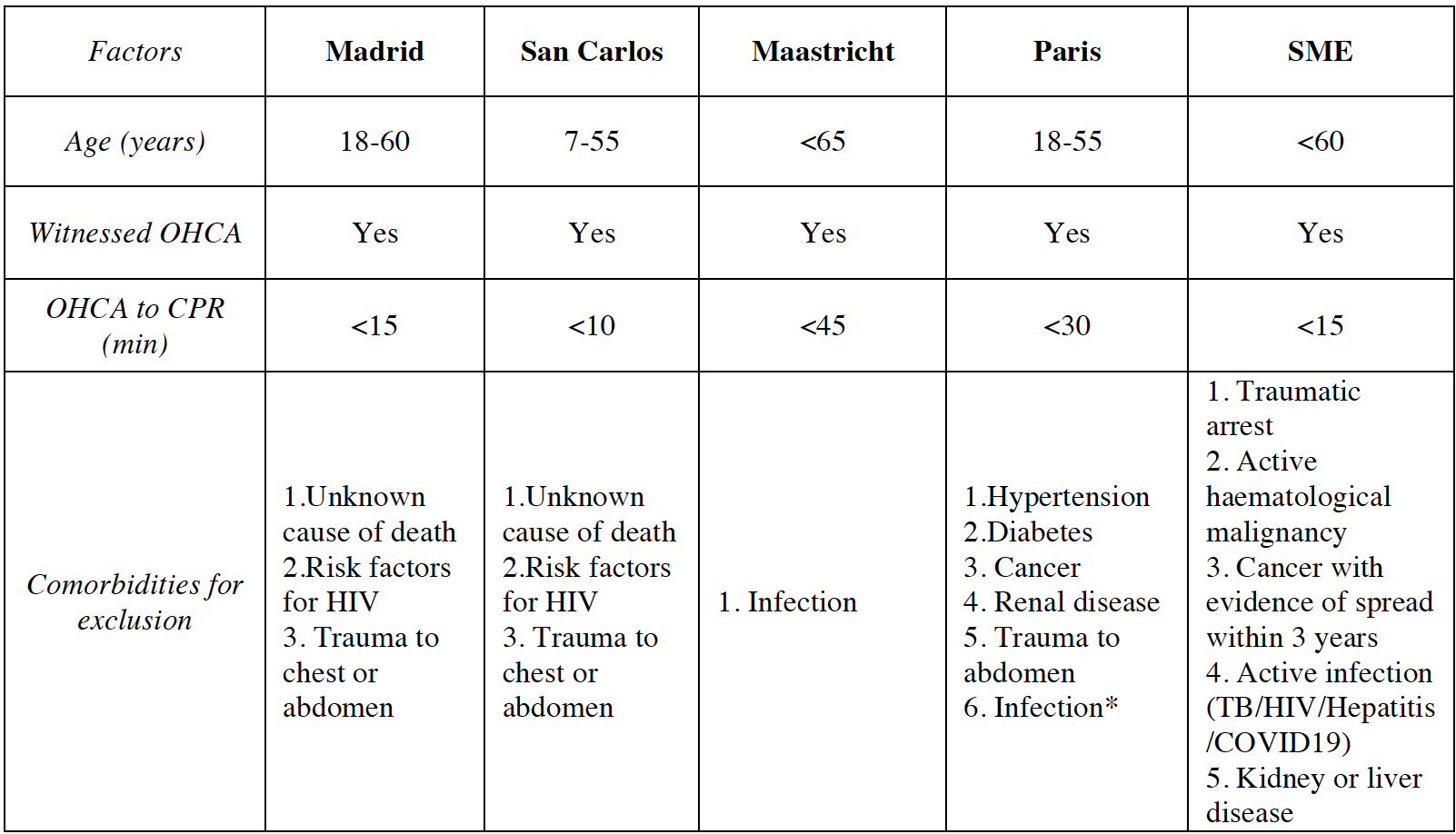
Methods: A retrospective observational cohort study was conducted, using data from the Canadian Resuscitation Outcomes Consortium (canROC) registry. Consecutive OHCA cases from January 1, 2016 to December 31, 2018 were analyzed. Five sets of international uDCD criteria (including one informed by local subject matter experts) were applied to the study population in order to approximate the potential donor pool within this OHCA population. This study sought to identify a range of potential, based on several best and worst case scenarios.
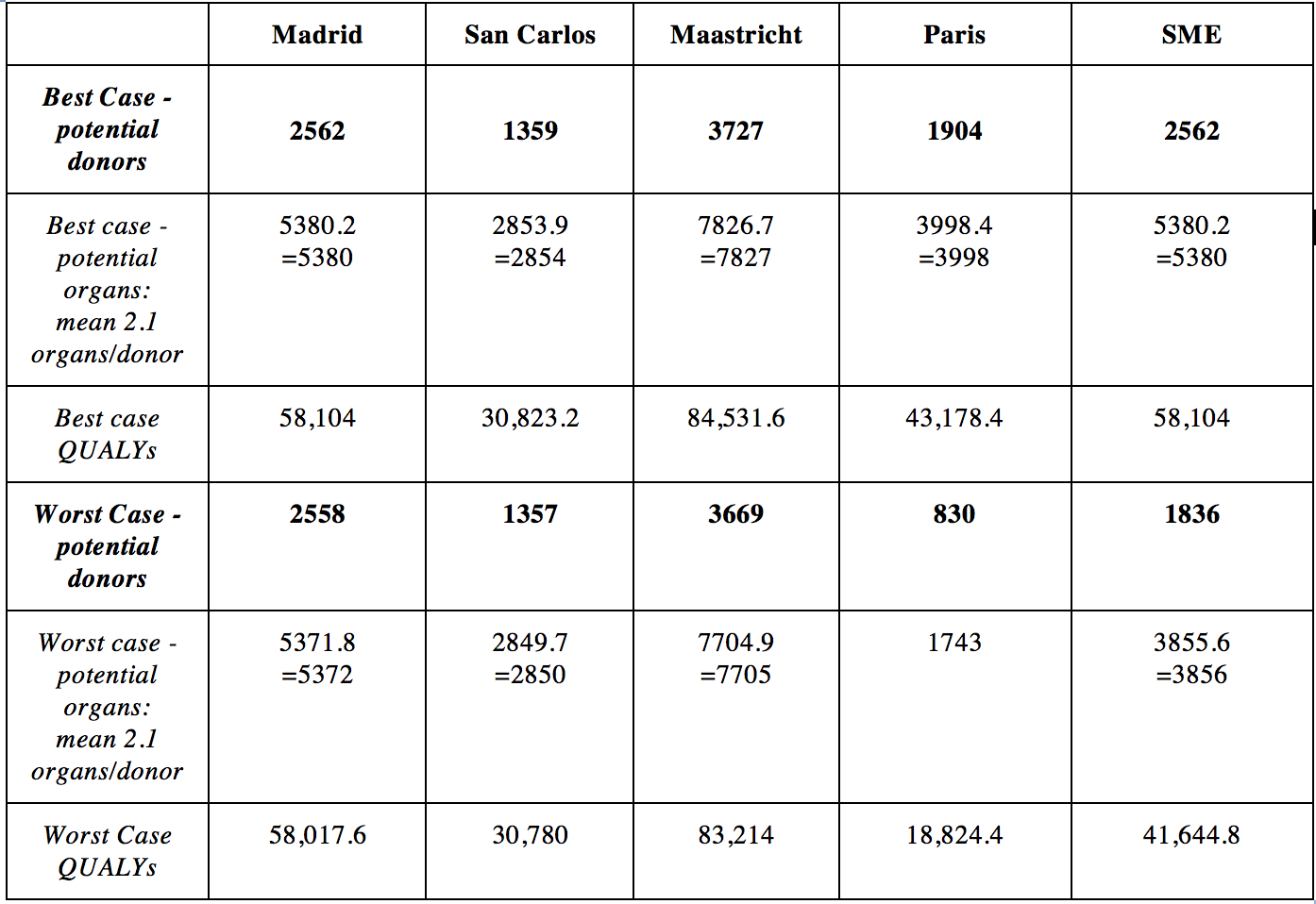
Results: Of 33,076 OHCA cases, a total study population of 9353 was identified. Of these, 4331 were not transported to hospital after resuscitation. A range of 830 to 3727 potential donors were identified (depending on uDCD criteria applied), translating to an additional 1743 to 7827 organs retrieved per year (based on 2.1 organs per donor) and representing a range of 18,824.4 to 84,531.6 Quality Adjusted Life Years (QALYs) for potential recipients.
Conclusions: Utilizing the OHCA population in uDCD pathways could have a significant impact on organ transplant waitlists in Canada. This study demonstrates the viability of the adult OHCA population to increase the potential donor pool with uDCD, which could also have large financial and economic impacts. However, creating and implementing such programs would face challenging logistical, geographical, medical-legal and ethical barriers, which would need to be addressed in order to contribute to meaningful change. This study is an important foundational step in the development of a program of research to understand and identify the potential for uDCD after OHCA in Canada.