Six-month long monitoring of cerebral blood perfusion evolution by computed tomography angiography, computed tomography perfusion and transcranial Doppler sonography in an infant suffering post-anoxic brain damage after intrauterine circulatory arrest, primarily demonstrating death by neurological criteria symptoms later followed by two weeks delayed recovery of respiratory drive - case report
Romuald Bohatyrewicz1, Łukasz Zwarzany2, Wojciech Walas3, Katarzyna Chamier-Ciemińska2, Joanna Sołek-Pastuszka1, Klaudyna Kojder1, Filip Szeremeta4, Barbara Steinborn5, Małgorzata Mikaszewska-Sokolewicz6, Monika Bekiesińska-Figatowska7, Krzysztof Kochanek8, Joanna Wojczal9, Katarzyna Sznajder10, Wojciech Poncyljusz2, Marcin Sawicki2.
1Department of Anaesthesiology and Intensive Care, Pomeranian Medical University in Szczecin, Szczecin, Poland; 2Department of Diagnostic Imaging and Interventional Radiology, Pomeranian Medical University in Szczecin, Szczecin, Poland; 3Department of Anaesthesiology and Intensive Care, Institute of Medical Science, University of Opole, Opole, Poland; 4Department of Anaesthesiology and Intensive Therapy, Silesian Hospital in Cieszyn, Cieszyn, Poland; 5Department of Developmental Neurology, Poznan University of Medical Sciences, Poznań, Poland; 6Clinic of Anaesthesiogy and Intensive Care, The Children Memorial Health Institute, Warszawa, Poland; 7Department of Diagnostic Imaging, Institute of Mother and Child, Warszawa, Poland; 8Institute of Physiology and Pathology of Hearing, Warszawa, Poland; 9Department of Neurology, Medical University of Lublin, Lublin, Poland; 10Clinical Department of Diagnostic Imaging, Institute of Medical Sciences, University of Opole, Opole, Poland
CASE REPORT: Exceptionally rarely reported persistence or reappearance of respiratory activity in patients fulfilling the rest of death by neurologic criteria (DNC) symptoms often brings suspicion of incorrect diagnostic procedure. In this situation we would like to present a case of term female newborn admitted to paediatric intensive care unit (PICU) after intrauterine circulatory arrest. Initially implemented therapeutic hypothermia was terminated next day. Devastating brain injury was confirmed by magnetic resonance imaging (MRI), ultrasonography (USG) and computed tomography.
Two physical examinations conducted on days 9 and 13 confirmed brainstem areflexia and apnoea. It would allow DNC diagnosis based solely on clinical findings and ascertainment of devastating brain injury. This was not completed because of persisted cerebral blood flow (CBF) recognized in USG and computed tomography angiography (CTA). Futility of further therapy became obvious, but termination of ventilation in patients not declared dead is unacceptable in Poland. Therefore, limited therapy was continued and relatives accepted periodic monitoring of CBF and electrophysiological testing.
Third examination on day 27 confirmed brain stem areflexia, but in the 4th minute of apnoea test shallow breaths were noticed and the test was terminated. Since that moment respiratory activity was gradually increasing but no brainstem reflexes were recorded until the end of patients stay in PICU.
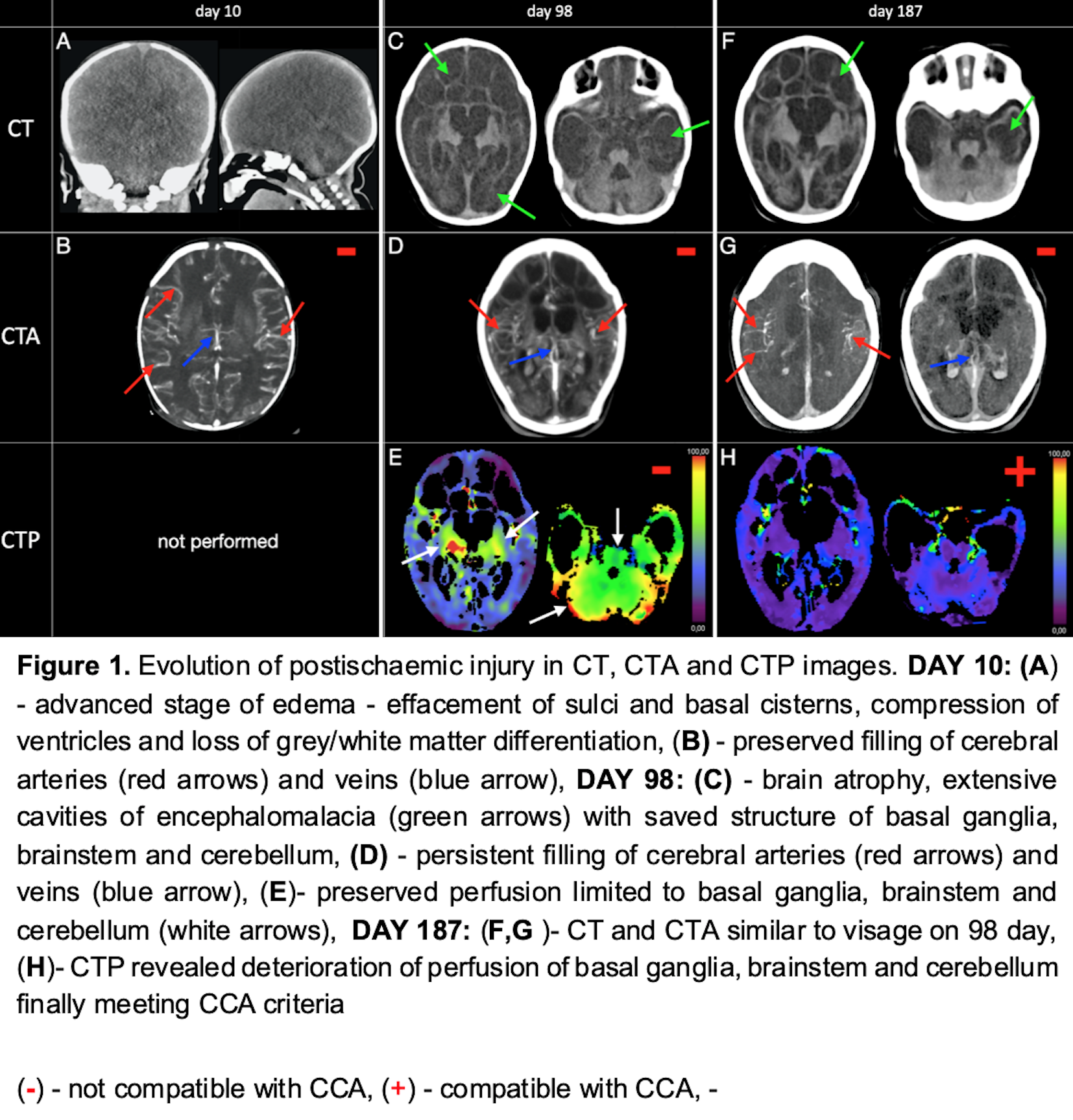
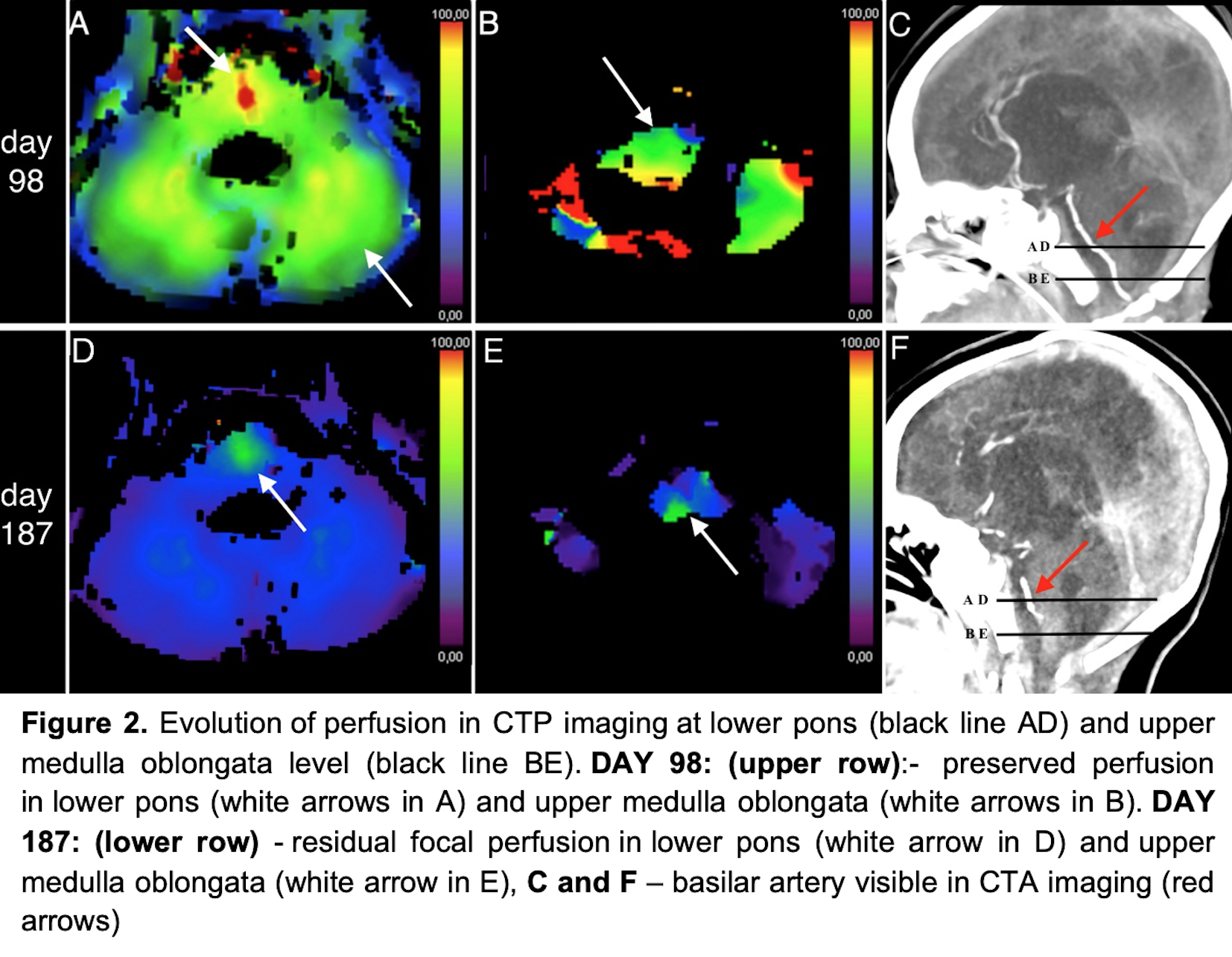
CBF examinations in paediatric patients demonstrating DNC symptoms were approved by Bioethical Committee. Summary of CTA and CTP performed on day 10, 98 and 187 is demonstrated in Figures 1 and 2. CTA recorded persisted CBF in all three examinations while CTP recorded persisted CBF on days 10 and 98 and cerebral circulatory arrest (CCA) on day 187. Despite absence of CBF in all routinely analyzed regions of interest we noticed in this third examination small area of persisted perfusion in close proximity to basilar artery which is corresponding with respiratory centre localization.
The other ancillary tests presented results as follows: EEG – days 10, 25, 96 and 161 – persisted activity; auditory evoked potentials – day 12 – persisted activity, day 149 – inconclusive; transcranial Doppler – day 86 – normal CBF.
On day 271 patient was transferred to palliative unit where she died 5 days later.
CONCLUSION: Our observation suggests that in extremely rare cases respiratory drive may persist or recover even if minimal part of brainstem remains perfused. This might be similar to limited restitution of neuronal functions following ischaemic stroke.
Careful explanation of these mechanism to the family may help to avoid serious misunderstandings.