Are race & ethnicity factors in determining organ procurement organization response to potential donors and families? Results from a single OPO
Thomas Mone1, J. Thomas Rosenthal MD2, Tom Seto3, Rosemary O'Meeghan MD4.
1Administration, OneLegacy, Azusa, CA, United States; 2Governing Board, Administration, Organ Operations, OneLegacy, Azusa, CA, United States; 3Information Technology, OneLegacy, Azusa, CA, United States; 4Organ Operations, OneLegacy, Azusa, CA, United States
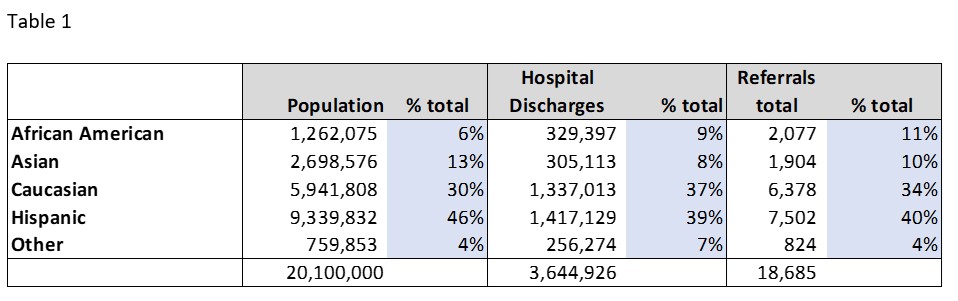
Purpose: It has been asserted that organ procurement organizations (OPOs) use race and ethnicity to determine whether to respond to referrals and approach families for donation and thereby contribute to transplantation inequity. These concerns have not yet been addressed with data by OPOs. The purpose of this study was to use a robust electronic donor record that automatically captures all interactions with donor hospitals, including personnel time, to assess whether race is a factor in critical donation processes.
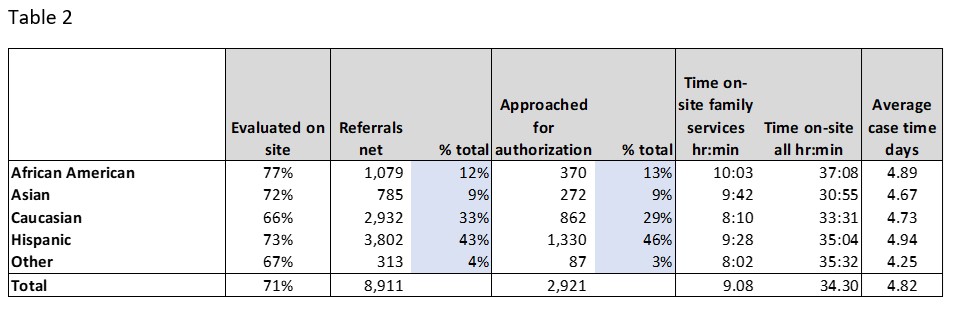
Given the possible harm done to public trust in donation by recent public discussion on race, OPOs’ reporting their data on racial equity, even if one at a time, would help assure individual and community trust, which are essential for continued improvement.